Transcranial Magnetic Stimulation
By Hudson Mind
Introducing TMS
Transcranial Magnetic Stimulation (TMS) is a breakthrough in the treatment landscape for major depression and OCD. Originally introduced in 1985, the power of TMS is supported by more than 30 years of clinical research. Since its inception, TMS has consistently delivered relief from symptoms in patients who have tried psychotherapy and antidepressant medications to no avail.
The complexity of depression is underestimated. Researchers are still exploring new layers of the physiology of depression in the brain. One aspect of depression that is assured is that it is not a one-size-fits-all condition. As we continue to learn about underlying roots and correlations, we know that we have to innovate treatments that extend beyond the barriers of conventionality —barriers that have left too many people behind and struggling to find relief and hope.
TMS fills this void.
A chemical-free and non-invasive solution, TMS technology uses magnetic fields to re-activate neural activity within brain structures that are related to major depression.
TMS is a product of a new mental health era—one that finally recognizes the complexity of the brain and explores solutions that work through that complexity, not around it.
A Closer Look at Depression
Before we break down the science behind TMS, it’s important to understand what is happening in the brain of someone living with treatment-resistant depression.
It is estimated that 5% of adults across the globe live with depression. While the catalysts for depression can vary greatly—and include genetics, environment, life events, medical conditions, or psychiatric disorders—there are consistencies among the physiological outcomes of depression in the brain.
A healthy brain and a depressed brain look different. And that’s because depression actually has the power to alter neural structures.
Within a healthy brain, neurotransmitters can seamlessly deliver signals and messages between brain cells. But their efficiency starts to break down in a depressed brain, which means that the brain of a person living with major depression struggles to consistently send and receive messages that help to regulate mood. It is this loss of synaptic connection that clinical researchers believe contribute to the composition of depression.
This more comprehensive vision of depression in the brain has given way to the development of breakthrough treatments, like TMS.
Who can benefit from TMS?
TMS is an especially effective solution for anyone who has what is known as treatment-resistant depression. Meaning, that symptoms of depression (or OCD and smoking addiction) have not improved after trying chemical medication or talk therapy.
It’s also an optimal treatment route for people who want to feel relief from their symptoms without the risk of experiencing detrimental side effects that are common to antidepressant medication.
TMS treatment also makes it possible to continue living your life. Some other types of treatment require patients to essentially put their daily activities on hold. But each TMS treatment can be completed in under 20 minutes and because there are no serious side effects, you have the freedom to return to your daily plans as soon as your treatment is over.
The Science (How TMS Works)
TMS uses MRI-strength magnetic pulses to reactivate and regulate neurotransmitters that have lost function due to chronic stress and depression in the brain. Through magnetic stimulation, neurotransmitters that had been deficient or dormant, are essentially revived.
The pulses also activate synaptic plasticity and neurogenesis in the hippocampus region, which enhances the communication between separate regions of the brain.
The pulses emanate from a helmet that contains electro-magnetic coil configurations that target mood-regulating regions of the brain. Depending on the type of coil design (more on that below), TMS treatments can target specific regions of the brain related to either depression, OCD, or smoking addiction. The latest development of TMS technology has introduced coil designs that specifically focus electromagnetic pulses on either the Dorsolateral prefrontal cortex.
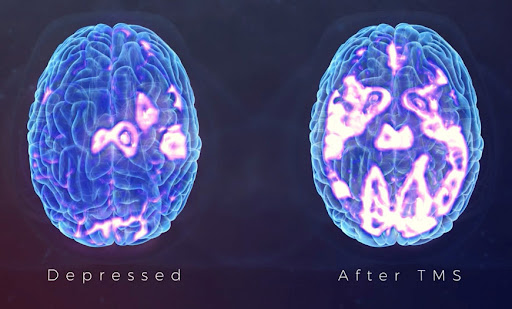
TMS essentially reboots the depressed brain’s interconnected messaging system, making it possible to receive new messages and forge new neural connections—connections that can help break free from a cycle of depressive thoughts and moods.
What else can TMS treat?
OCD
TMS is an effective solution for diminishing the obsessive thoughts and compulsive behaviors that contribute to Obsessive-Compulsive Disorder (OCD). More prolific OCD treatments like cognitive behavioral therapy and exposure therapy focus on helping patients learn how to refrain from acting on their compulsions.
TMS, however, is focused on regulating the neural activity associated with OCD.
TMS concentrates magnetic stimulation to specific regions of the brain (medial prefrontal cortex and anterior cingulate cortex) to decrease impulses at the root.
TMS concentrates magnetic stimulation to specific regions of the brain (medial prefrontal cortex and anterior cingulate cortex) to decrease impulses at the root.
Smoking addiction
TMS is also FDA-cleared and clinically-proven to assist with smoking cessation. By emitting electromagnetic pulses at the bilateral insula and prefrontal cortex regions of the brain, TMS is able to stimulate neurons that are proven to reduce tobacco cravings and strengthen impulse control.
Following a four-week study, 28% of Deep TMS participants had successfully quit smoking.
The Technology
At Hudson Mind, we utilize Deep TMS technology to help our patients achieve even more targeted results. Deep TMS is an evolution from the electromagnetic coil design first developed for Traditional TMS treatments.
Traditional TMS
Traditional TMS treatments utilize a figure-8 shaped coil that is limited in its ability to target depth and breadth. Traditional TMS figure-8 coils are also only capable of targeting symptoms of depression due to the shape at which the pulses are emitted. Typically, a figure-8 coil can reach a depth of .7 cm to 1.1 cm in the brain.
Deep TMS
To activate neurons in depressed brains, Deep TMS technology utilizes a patented H1 coil design to target brain regions related to depression with more precision, depth, and scope. The technology also features a separate coil configuration designed specifically to activate neurons in brain regions associated with OCD.
Compared to standard TMS technology, Deep TMS coils can reach anywhere from 1.8 cm to 3.5 cm in depth. Because both of these coil designs cover more surface area, more neurons are stimulated, which means that the odds of missing specific neural pathways diminish greatly.
Courses of Treatment
The efficacy of Deep TMS is staggering. But in order to feel lasting relief from symptoms, and revive the neurocircuitry in regions of the brain, patients are encouraged to complete a full treatment. Here at Hudson Mind, we offer two different TMS paths: Standard and Accelerated.
Standard
36 treatments are administered once per day over the course of 8 to 10 weeks (36 total), depending on your specific diagnosis protocol. Each treatment duration ranges from 8-22 minutes.
Standard TMS is FDA-cleared and accepted by most insurance carriers as long as certain clinical requirements are met.
For a list of contraindications and in-network carriers, please see FAQ.
Accelerated
Treatment is delivered through a fixed, condensed/rapid schedule. Over the course of 5 days, you will receive 50 treatments (10 treatments per day, each spaced out by 50 minutes).
Accelerated programs are not covered by insurance and cash-pay only.
Saint Protocol: Stanford Accelerated Intelligent Neuromodulation Therapy
A recent groundbreaking study at Stanford University found that a series of accelerated rapid TMS treatments spread out over consecutive days had significant results in remission rates. At Hudson Mind we are proud to model our accelerated treatment modeled off of the SAINT Protocol.
What is a typical treatment session like?
Pre-treatment
Before scheduling any treatment, we will first have you fill out a clinical intake questionnaire which will ask you for information such as your symptoms, medical history and past/current medications. A provider will review this with you in your TeleHealth evaluation, which will be the first step as a new Hudson Mind patient. Once cleared for treatment (and if going through insurance, we get a prior authorization) then we can start scheduling immediately.
Brain mapping
During your first session our technician will perform a “brainmap.” A brainmap is exactly what it sounds like: a map of your brain. The technician will place a helmet with coils inside on your head and send single pulses to your motor cortex. These pulses do not hurt—most people say they feel like a light tap on the outside of the helmet. The purpose of these pulses is to prompt involuntary movement in your hand or foot (depending on the part of the brain that needs to be stimulated). Based on the strength of your involuntary reactions, the technician will be able to precisely determine the coordinates of your brain they need to target in subsequent TMS sessions.
TMS session
During each TMS session, the technician will first place the coil helmet on your head to measure your motor threshold, . After ensuring comfort and correct placement, the technician will start the pulses. The pulses may last anywhere from 8-22 minutes in a standard treatment session.
If you’re getting treatment for symptoms of depression, we recommend bringing materials that will elevate your mood. The materials can range from books, pictures, a meditation app, a playlist of your favorite songs or YouTube videos. And you don’t have to bring the same thing every time. You can experiment to see which materials put you into a more relaxed headspace. And don’t feel pressure to bring something in if you’re not comfortable. Some people actually prefer to chat with the technician throughout their session.
For OCD treatment, your sessions will begin with the technician playing a series of provocations that have been previously designed for you by a therapist. The point of these provocations is to provoke you to a certain level of distress right before the session begins.
Cost
For more information on pricing, please view our list of rates here.
How to prepare for treatment
While undergoing TMS treatment, it’s important to keep everything as consistent as possible. Keep your sleep patterns, caffeine intake and medication regimen the same throughout your TMS course. Any deviations from this schedule should be reported to your technician/prescribing provider. Alcohol consumption should ideally be limited during treatment, especially any binge drinking.
Common Questions
Everybody’s mental healing journey is different, and that’s okay. TMS might be for you if you have not felt significant relief from medications and/or psychotherapy.
Yes! You can continue taking your prescription once you begin TMS. Actually, we recommend it. Always be sure to communicate any dosage or medication changes with our team.
Every body is different. You might notice improvement in mood within the first few weeks of starting treatment, or you may not feel any change until the completion of treatment.
Great question. Here are the facts:
At Hudson Mind, we use BrainsWay’s cutting-edge Deep TMS technology. Research shows that for patients receiving Deep TMS treatment, 64% showed a positive response after 20 sessions, with 42% of patients meeting remission criteria. After about 30 sessions, 75% of patients showed a positive response, with 51% meeting remissions criteria. We will never make guarantees, but the data is very promising.
At Hudson Mind, we use BrainsWay’s cutting-edge Deep TMS technology. Research shows that for patients receiving Deep TMS treatment, 64% showed a positive response after 20 sessions, with 42% of patients meeting remission criteria. After about 30 sessions, 75% of patients showed a positive response, with 51% meeting remissions criteria. We will never make guarantees, but the data is very promising.
Results tend to vary from patient to patient. But studies do show that patients who experience a significant reduction in symptoms are more likely to show continued positive response from anywhere between six months to one year after completion of treatment.
If your insurance covers TMS, it may reauthorize treatment after a six-month period in case any maintenance is needed.
If your insurance covers TMS, it may reauthorize treatment after a six-month period in case any maintenance is needed.
Yes, in order to be covered for TMS, you must not have any of the following contraindications:
–No active suicidal ideation
–No psychotic symptoms
–No metal in your cranium
–No neurological conditions (seizures/TBI/brain tumors)
–No active substance abuse
-No diagnosis of bipolar disorder
It is worth noting that while these rule-out insurance coverage, it doesn’t mean you can’t get TMS at all. During the consultation, our providers will determine if TMS is safe for you.
–No active suicidal ideation
–No psychotic symptoms
–No metal in your cranium
–No neurological conditions (seizures/TBI/brain tumors)
–No active substance abuse
-No diagnosis of bipolar disorder
It is worth noting that while these rule-out insurance coverage, it doesn’t mean you can’t get TMS at all. During the consultation, our providers will determine if TMS is safe for you.
As long as it was only a one-time seizure and you have not had any episodes since, and are not currently on antiepileptic medications, TMS is safe for you. Please discuss this with our team during your consultation.
If you feel any discomfort, it is okay to take over-the-counter pain relievers, like Tylenol or Advil. You can also take over-the-counter pain relievers before you come in for an appointment to mitigate any discomfort. Side effects tend to decrease over time, especially as your body gets acclimated to treatment.
You can safely receive TMS treatments throughout your pregnancy, and research shows successful results among pregnant people. However, you should know that insurance will not cover treatment for you if you are pregnant.
It’s always a good idea to connect with your provider if you are pregnant, or may become pregnant.
It’s always a good idea to connect with your provider if you are pregnant, or may become pregnant.
Standard TMS is FDA-cleared and accepted by most insurance carriers as long as certain clinical requirements are met. Insurance requirements vary by carrier, but they typically look for a history of between two and four failed antidepressants, as well as failed trials of therapy. In-network carriers include: Aetna, Affinity, Empire BCBS, Cigna, HealthFirst, Medicare, United Healthcare, 1199.
Accelerated TMS is considered off-label, and therefore not covered by insurance.
Accelerated TMS is considered off-label, and therefore not covered by insurance.
We want to ensure this treatment is as accessible to you as possible, and we will certainly do the leg work with insurance carriers and advocate on your behalf. But there may be some plans that are not willing to cover treatment at all due to specific diagnoses or contraindications.
If you think you might be eligible for financing options due to a documented financial hardship, please fill out this eligibility form and a Patient Services Representative will reach out shortly.
Yes! TMS for depression is covered by both Medicare/Medicaid as long as you meet certain clinical requirements:
1) You have been clinically diagnosed with depression.
2) You have completed antidepressant trials with no significant results.
3) You have completed therapy trials with no significant results.
*Please note: Fidelis Medicaid plan does not cover TMS.
1) You have been clinically diagnosed with depression.
2) You have completed antidepressant trials with no significant results.
3) You have completed therapy trials with no significant results.
*Please note: Fidelis Medicaid plan does not cover TMS.
We have both Deep TMS and Traditional TMS machines on-site.Following your complimentary educational screening, our team will determine which treatment is right for you.
- Noohi S, Amirsalari S. History, Studies and Specific Uses of Repetitive Transcranial Magnetic Stimulation (rTMS) in Treating Epilepsy. Iran J Child Neurol. 2016 Winter;10(1):1-8. PMID: 27057180; PMCID: PMC4815479.
- “What Is Depression?: Anxiety and Depression.” What Is Depression? | Anxiety and Depression, https://adaa.org/understanding-anxiety/depression.
- “How Depression Affects the Brain.” Yale Medicine, Yale Medicine, 17 June 2021, https://www.yalemedicine.org/news/neurobiology-depression.
- Horovitz, Naama. “Deep TMS as Anterior Cingulate Cortex-Focused OCD Treatment.” BrainsWay, 12 Aug. 2021, https://www.brainsway.com/knowledge-center/deep-transcranial-magnetic-stimulation-of-the-anterior-cingulate-cortex-in-obsessive-compulsive-disorder-patients/.
- News Center. “Experimental Depression Treatment Is Nearly 80% Effective in Controlled Study.” News Center, 28 Oct. 2021, https://med.stanford.edu/news/all-news/2021/10/depression-treatment.html.
- Hudson Mind research: Transcranial Magnetic Stimulation—The Science
- McCarter, Thomas. “Depression overview.” American health & drug benefits vol. 1,3 (2008): 44-51.
- Chand SP, Arif H. Depression. [Updated 2021 Jul 26]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2021 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK430847/
- Duval, Fabrice et al. “Treatments in depression.” Dialogues in clinical neuroscience vol. 8,2 (2006): 191-206. doi:10.31887/DCNS.2006.8.2/fduval
- Ramic, Enisa et al. “Assessment of the Antidepressant Side Effects Occurrence in Patients Treated in Primary Care.” Materia socio-medica vol. 32,2 (2020): 131-134. doi:10.5455/msm.2020.32.131-134
- Chail, Amit et al. “Transcranial magnetic stimulation: A review of its evolution and current applications.” Industrial psychiatry journal vol. 27,2 (2018): 172-180. doi:10.4103/ipj.ipj_88_18
- Stultz, Debra J et al. “Transcranial Magnetic Stimulation (TMS) Safety with Respect to Seizures: A Literature Review.” Neuropsychiatric disease and treatment vol. 16 2989-3000. 7 Dec. 2020, doi:10.2147/NDT.S276635
- Zhang, Fei-Fei et al. “Brain structure alterations in depression: Psychoradiological evidence.” CNS neuroscience & therapeutics vol. 24,11 (2018): 994-1003. doi:10.1111/cns.12835
- Post, A, and M E Keck. “Transcranial magnetic stimulation as a therapeutic tool in psychiatry: what do we know about the neurobiological mechanisms?.” Journal of psychiatric research vol. 35,4 (2001): 193-215. doi:10.1016/s0022-3956(01)00023-1
- Brigitta, Bondy. “Pathophysiology of depression and mechanisms of treatment.” Dialogues in clinical neuroscience vol. 4,1 (2002): 7-20. doi:10.31887/DCNS.2002.4.1/bbondy
- Avery, et al. (2008). Transcranial Magnetic Stimulation in the Acute Treatment of Major Depressive Disorder: Clinical Response in an Open-Label Extension Trial. J Clin Psychiatry, 69 (3):441-451.
- Sackeim HA, et al. (2020). Clinical Outcomes in a Large Registry of Patients with Major Depressive Disorder Treated with Transcranial Magnetic Stimulation. J Affective Disorders, 277(12):65-74.
- Dunner, David L et al. “A multisite, naturalistic, observational study of transcranial magnetic stimulation for patients with pharmacoresistant major depressive disorder: durability of benefit over a 1-year follow-up period.” The Journal of clinical psychiatry vol. 75,12 (2014): 1394-401. doi:10.4088/JCP.13m08977
- Carpenter, Linda L et al. “Transcranial magnetic stimulation (TMS) for major depression: a multisite, naturalistic, observational study of acute treatment outcomes in clinical practice.” Depression and anxiety vol. 29,7 (2012): 587-96. doi:10.1002/da.21969
- Janicak, Philip G et al. “Durability of clinical benefit with transcranial magnetic stimulation (TMS) in the treatment of pharmacoresistant major depression: assessment of relapse during a 6-month, multisite, open-label study.” Brain stimulation vol. 3,4 (2010): 187-99. doi:10.1016/j.brs.2010.07.003
- Janicak, Philip G, and Mehmet E Dokucu. “Transcranial magnetic stimulation for the treatment of major depression.” Neuropsychiatric disease and treatment vol. 11 1549-60. 26 Jun. 2015, doi:10.2147/NDT.S67477
- O’Reardon, John P et al. “Efficacy and safety of transcranial magnetic stimulation in the acute treatment of major depression: a multisite randomized controlled trial.” Biological psychiatry vol. 62,11 (2007): 1208-16. doi:10.1016/j.biopsych.2007.01.018
- McGrath, Patrick J et al. “Tranylcypromine versus venlafaxine plus mirtazapine following three failed antidepressant medication trials for depression: a STAR*D report.” The American journal of psychiatry vol. 163,9 (2006): 1531-41; quiz 1666. doi:10.1176/ajp.2006.163.9.1531
Back to the Top
Break Free
Contact us to schedule your complimentary consultation.